We are very excited to share some big news!
In our new study published in Nature last month, we uncover the mechanism through which inflammatory monocytes stimulate CD8+ T cells within the tumour microenvironment (TME) and how cancer cells can evade this anti-tumour immunity.
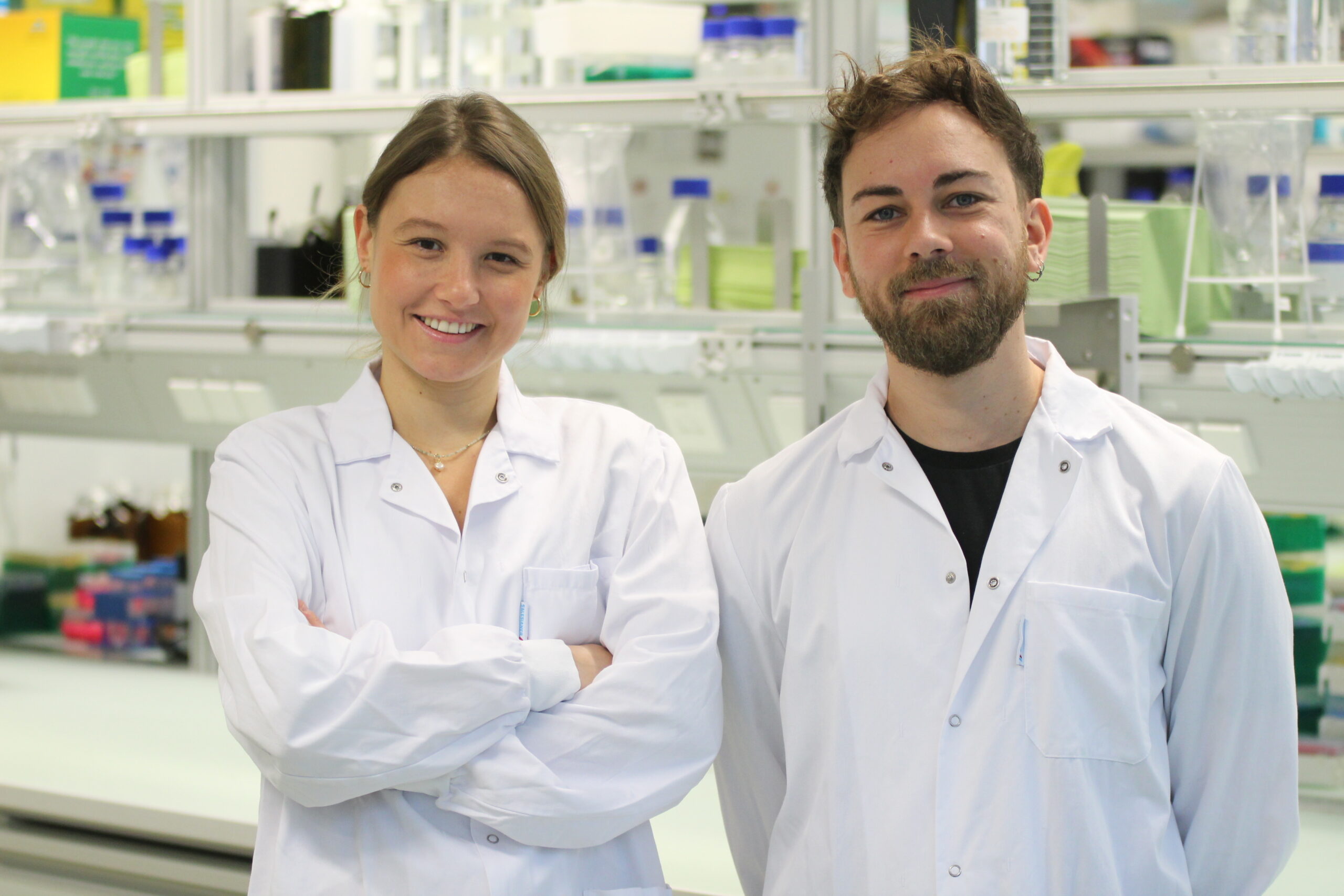
In an incredible effort led by amazing PhD students Anais and Guillem, we interrogate two immuno-oncology questions: How are CD8+ T cells restimulated in the TME and how do cancer cells disrupt this process? The authors leverage clinically relevant mouse models, functional genetics, imaging technologies, and single cell sequencing to gain a mechanistic insight into these processes.
It is well known that T cells rely on activation by antigen-presenting cells (APCs) such as dendritic cells (DCs) to be able to recognise and destroy cancer cells. However, the role of other immune cells, such as monocytes, has been overlooked for many years.
Using two mouse melanoma models- one naïve to targeted therapy and immunotherapy (NTT) and a second cross-resistant to both treatments (RTT), the authors first show that inflammatory monocytes are abundant in NTT tumours but not RTT tumours. The first exciting finding was that these inflammatory monocytes, characterised by high levels of IFN-stimulated genes (ISGs), can stimulate T cells through peptide MHCI cross-dressing and reactivate them within the TME. This T cell restimulation within the TME, is essential to the full effectiveness of the T cells.
In contrast, RTT tumours were characterised by an abundance of suppressive macrophages and only a few inflammatory monocytes. We recently showed that the immunosuppressive TME in the RTT model is shaped by oncogenic MAPK signaling with increased transcriptional output in cancer cells. Building on this work we were now able to identify two immune evasion mechanisms in RTT tumours: increased PGE2 production and reduced type I interferon production.
We demonstrate that these mechanisms prevent monocytes from acquiring an inflammatory state instead pushing them to differentiate to immunosuppressive macrophages, thus effectively preventing T cell restimulation. Blocking PGE2 production (through COX1/2 gene deletion) or restoring IFN-I signaling (through IRF3 and IRF7 overexpression) in RTT tumors was sufficient to restore T cell responses and tumor control through the activation of monocytes, even in the absence of DCs.
Based on these insights, we developed combination therapies with COX2 inhibitors (to block PGE2), 5-Azacitidine (to boost IFN-I) and Flt3L (to expand antigen-presenting cells), aiming to improve the outcome of immunotherapies. The combinations showed encouraging results across multiple pre-clinical resistant tumor models, including melanoma, lung, colorectal and pancreatic cancers suggesting broad therapeutic potential.
Continuous treatment with COX2 inhibitors is needed to maintain the permissive immune microenvironment as when treatment is stopped, tumors can quickly relapse. This highlightings the dynamic nature of immune responses and the continuous requirement for a stimulatory TME.
Our findings help explain why NSAID use (which block PGE2 production) correlates with better immunotherapy responses in melanoma and lung cancer patients. Additionally, they open new therapeutic avenues, targeting both the PGE2 and IFN-I pathways and show how monocytes can be promising targets to boost immunotherapies.
Our goal is to deepen the mechanistic understanding of anti-tumour immunity and so future research will focus on exploring how stimulating T cells with monocytes and other immune cells plays out in different forms of immunotherapy. This knowledge could reveal new avenues to overcome resistance to immunotherapies, rendering them a viable option for a broader range of patients.
To learn more you can follow:
For the full paper : www.nature.com/articles/s41…
Summary on bluesky
Institute annoucement: https://www.imp.ac.at/news/article/a-turning-point-for-cancer-treatment-monocytes-boost-t-cells-in-immunotherapy